Following the covid eruption, you may have come across the terms disinfection, sterilization, and even sanitisation at regular intervals. All of these phrases refer to antimicrobial procedures aimed at eradicating pathogenic microorganisms and other infectious agents.
Disinfection is a common and simple method of decontamination that we employ on a daily base. On the other hand, sterilization is predominantly linked with medical, industrial, and scientific areas and is not performed very frequently for household purposes.
Sterilization can be thought of as the most advanced approach for ensuring the elimination of all pathogenic living forms. In contrast, disinfection just decreases the germ count to a non-threatening level rather than entirely removing them.
However, you must first understand the significant differences between these procedures before deciding which kind of asepsis is best for your situation. In the following context, we will try to point out the differences between sterilization and disinfection, including a quick description, types, and instances.
Content: Sterilization Vs Disinfection
Comparison Chart
| Basis of Comparison | Sterilization | Disinfection |
|---|---|---|
| Meaning | The process which assures the complete decontamination with infectious pathogens, bacterial or vegetative spores etc by using highly technical and scientific approaches. | The process which reduces microbial count upto a non-threatening level but doesn't eliminate them completely. |
| Applications | In medical sector, food & pharmaceutical industries, research labs etc. | In industries, households or public spaces for cleaning floors, machines and surfaces. |
| Examples | Autoclave, Hot air oven, Ethylene oxide gas, Membrane filtration, U.V. sterilization, etc. | Chlorination, Ozone treatment, hydrogen peroxide, alcohol treatment, etc. |
| Types | Heat, chemical, filtration, irradiation and high-pressure treatment. | Detergents, heavy metals, hydrogen peroxide, phenolic disinfectants etc. |
| Level of asepsis | Extreme level as it kills almost all the infectious living and non-living entities. | Adequate or average level as it lacks the ability to destroy the bacterial spores. |
| Chemistry behind | Kills, inactivates or eliminates all forms of microbes providing complete sterility. | Reduces the microbial count but doesn't eliminate them entirely. |
| Decontamination from spores | Possible to kill bacterial as well as vegetative spores. | Not possible to destroy any type of spore. |
| Risk Factor | Reduces the risk of infection by eliminating all contaminating factors. | Risk of infection is certainly high as it doesn't guarantee to kill all contaminants. |
| Strictness for Protocol | Has to abide the strict protocol otherwise there are chances of failure. | Strict protocol is not needed. |
| Contact Time | More contact time is necessary for successful sterilization as compared to disinfection. | Disinfection require adequate time as per the material to be sterilised. |
Why is disinfection or sterilization necessary?
We are surrounded by a plethora of microflorae. For instance, a gram of dirt has approximately 40 million bacteria, and a human mouth carries more bacteria than the whole world population. It is evident from this that microorganisms are an inseparable and unavoidable part of our lives.
The majority of microorganisms live in peace; however, some are hazardous to human health. For the sake of a healthy lifestyle, these hazardous pathogenic florae must be eradicated. Disinfection and sterilization are procedures used to clean the air, water, and surfaces in order to remove them.
Definition of Disinfection
“The antimicrobial process that targets to reduce the quantity of undesirable contaminating microbial fauna to a non-threatening level except for bacterial and vegetative spores is known as Disinfection.”
Disinfectants: Chemical substances which are used for disinfection are known as Disinfectants.
Examples of disinfecting agents
Alcohols
- Alcohol acts as a dehydrating agent which denatures cellular proteins.
- In the healthcare sector, alcohol generally refers to a mixture of two water-soluble chemicals-isopropyl alcohol and ethyl alcohol. These two are underrated germicidal compounds but are powerful disinfectants.
- Alcohol-based sanitisers are widely used for covid disinfection nowadays. For efficient sanitisation, the alcohol concentration in the sanitiser must be at least 70% (with 30% water).
Chlorine and Chlorine Compounds
- Chlorine-containing chemicals like hypochlorite are the most promising disinfectant choices.
- They are commonly utilised as they are accessible in both solid (e.g., calcium hypochlorite) and liquid (e.g., sodium hypochlorite) forms.
- The most preferred concentration of sodium hypochlorite is between 5.25%–6.15 %, which is often known as household bleach.
- The mechanism of action of these chlorine disinfectants has yet to be determined. Despite this, they remain popular due to their broad-spectrum antibacterial activity, hard water resistance, quick action, and cost-effectiveness.
Phenolic Compounds
- Phenols are used as disinfectants in a variety of settings, including the home, healthcare, laboratories, and industries.
- The phenol derivatives ortho-phenyl phenol and ortho-benzyl-para-chlorophenol are currently the most popular. This is due to the fact that they have improvised antimicrobial properties than the parent compound.
- Their mechanism of action varies with concentration. At greater concentrations, phenol acts as a protoplasmic poison that penetrates and disrupts the cell wall, ultimately precipitating the cell proteins. On the other hand, phenol with a lower concentration and higher molecular weight leads to the inactivation of essential enzymes and leakage of metabolites from the cell wall.
Hydrogen peroxide
- Hydrogen peroxide is considered risk-free, eco-friendly and safe for a sustainable environment. This is because, after disposal, it breaks down into natural elements like water and oxygen.
- H2O2 acts against a broad spectrum of microbial fauna, including viruses, bacteria, fungi, yeast etc. 0.5% concentration of hydrogen peroxide display viricidal and bactericidal activity within 1 minute while fungicidal activity in 5 minutes.
- Their mode of action is based on the formation of free radicals, which can destroy vital biological components such as lipids, DNA, and so on.
Iodophors
- Iodophors are iodine-based compounds that contain both disinfection and antiseptic properties. Its use is restricted to certain semi-critical medical equipment as it retains the stain and leaves an unpleasant odour.
- They have lethal effects on microorganisms as they penetrate directly inside the cell wall resulting in disruption of proteins and nucleic acids.
There are several other disinfectants like aldehyde derivatives, quaternary ammonia compounds, peracetic acids and so on. These all have their own advantages and disadvantages and are used at different places as per the condition.
Definition of Sterilization
“The antimicrobial technique used to eliminate any type of contamination, such as bacterial, fungal, and virus cells, as well as bacterial and vegetative spores, is called sterilization.”
In comparison to disinfection, sterilization is a highly technological approach for decontamination and cleansing. It necessitates specialised knowledge as well as specified equipment. It is a costly way of decontamination but is the most effective and promising way of ensuring environmental safety.
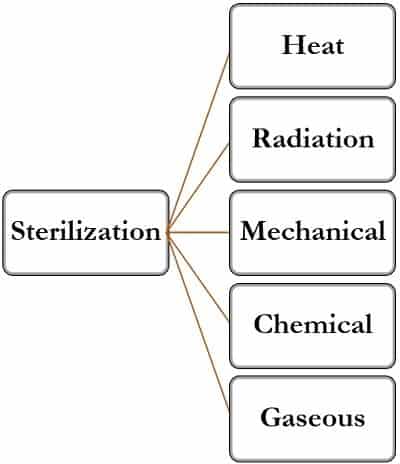
Types of Sterilization
The sterilization process can be classed into five categories:
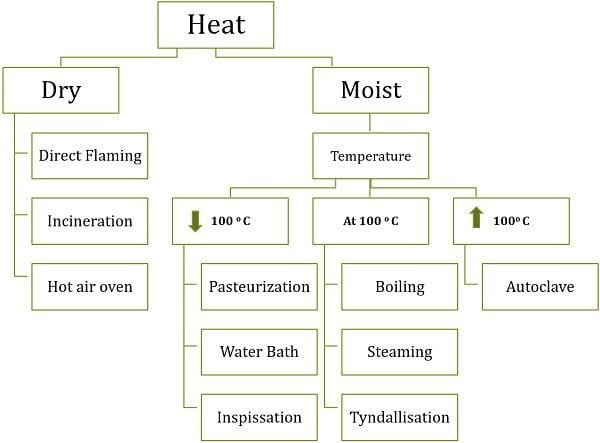
Heating Sterilization
Heating is one of the most ancient, simple and reliable methods of sterilization. It is highly preferred due to the following advantages:
- Kills all forms of microbes
- Cost-effective
- Non-time consuming
- Non-toxic
- Safe for the environment
Heating basically kills the microorganism by either coagulating or oxidising the protein components of a cell. This process of protein inactivation is called denaturation. A substance when is exposed to heat for a longer duration, the cellular components shrink, and the microbial cell eventually dies.
Heat sterilization can be employed in two ways:
- Moist heat sterilization
- Dry heat sterilization
Moist Heat Sterilization
Here the substance to be sterilised is subjected to hot water vapours or steam. This method generally coagulates the protein molecules leading to the deactivation of normal functioning inside the cell.
Moist heat sterilization can be achieved by the following techniques:
Below 100 oC
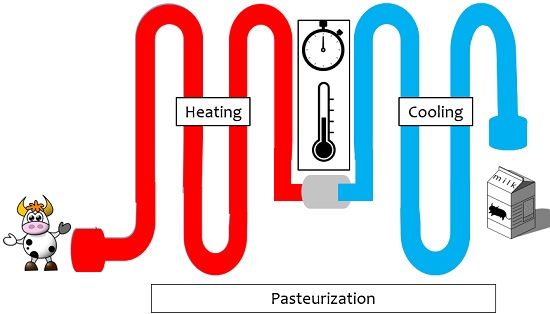
- Pasteurisation: This method is primarily associated with the sterilization of milk. Here, the milk is heated to higher temperatures (60-72 degrees) and then is cooled subsequently. This process of heating and cooling is repeated thrice or four times which kills the microbial fauna in the milk.
- Water bath: The water bath has a very simplified mechanism. The substances to be sterilised are kept inside and as the temperature rises, the heat inside the chamber rises too. They are used to sterilise serums, vaccines, culture media, body fluids etc.
- Inspissation: Inspissate refers to the process of making something thick by dehydration. This means to heat something for three consecutive days for 30 minutes at 80-90 o It is performed in an instrument known as Inspissator.
At 100 oC
- Boiling: It is the most trusted, convenient, accessible and user-friendly way of sterilization. Boiling is performed to sterilise household things as well as some healthcare tools.
- Steaming: It is an ordinary but effective way of sterilising. The substance to be sterilised is directly exposed to the steam. The hot steam kills the microbes on the surface.
- Tyndallisation: This technique was invented ‘John Tyndall‘. Its working mechanism is very much similar to inspissation. Here the equipment or the media are exposed to the steam at atmospheric pressure for about 90 minutes.
Above 100 oC
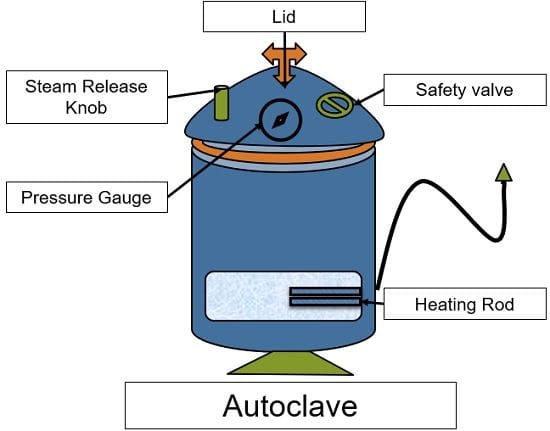
Autoclaving: This works with the principle of steam under pressure (121 oC; 15 lbs). The instrument used here is called an autoclave, which is a large vessel made of steel, wood or glass.
The autoclave is filled with water upto a certain level. As soon as this water boils, the steam is generated. This steam creates pressure in the chamber. The heat as well the pressure both kill the microbes effectively.
Dry Heat Sterilization
For thermally stable material, dry heat sterilization is preferred. During moist heat sterilization, some metallic equipment is at high risk of corroding due to moisture. Dry heat is the best option in these situations. Non-aqueous preparations, powders such as talc, porcelain goods, sharp metal tools, oils, fats, and other non-aqueous materials are commonly are sterilised by this.
It is performed in three common ways:
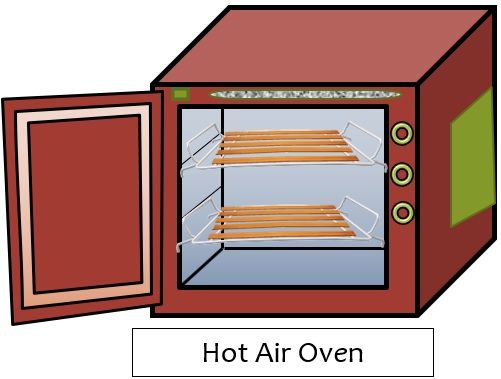
- Hot air oven: This is a steel and iron-clad closed chamber. It has a constant source of heat, raising the temperature inside the chamber. The objects held within are sterilised without becoming wet as a result of this method. It has temperature knobs to set the ideal temperature.
- Flaming: This is done for certain metallic or glass tools generally that are used in surgeries and culturing procedures. The object to be sterilised is directly exposed to flame, which destroys all microbial contaminants.
- Incineration: It is a peculiar technique that is used for organic medical debris like the placenta, body organs, pathogenic material etc. It is also used to reduce biohazardous substances into ash which decreases the volume of waste.
Here, the materials are subjected to direct flame at very high temperatures. It is based on the process of dry oxidation, which converts the organic debris into inorganic non-burnable material.
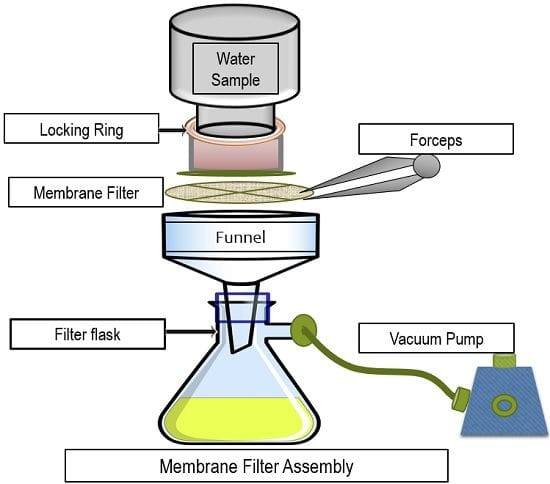
Mechanical Sterilization: Filtration
A cost-effective, intriguing, and user-friendly sterilization procedure that is mostly used to sterilise liquid materials such as water, drinks, and laboratory fluids.
Filtration is an effective method of sterilising heat-sensitive liquids. When a fluid passes through the filters, any unwanted particles are held inside. The liquid obtained at the bottom is sterilised quickly and easily.
It entails the use of several types of filters (pore size – 0.2 to 0.5 um) with varied pore sizes that are selected based on the substance to be sterilised.
Examples of some filters are:
| Type | Filter Used | Description |
|---|---|---|
| Membrane Filtration | Made up of cellulose | Traps the microbes larger than the pore size at the surface, filter is sensitive and gets ruptured easily used for online sterilization for injections, water purification etc. |
| Depth Filtration | Made up of three subsequent layers- | Microorganisms are trapped at the bottom of the filter bed, mainly used in water supply and sewage treatment plants. |
| a) cellulose fibres | ||
| b) diatomaceous earth | ||
| c) resin binder possessing charge. | ||
| Seitz Filtration | Made up of materials like asbestos | Filter is thicker than the membrane filter and thus don't get rupture during the filtration process. Major drawback- the filter absorbs a large volume of material during sterilization. |
| Sintered Glass Filtration | Made up of glass | Alternative to Seitz filtration, doesn't absorb the material. But are very sensitive and fragile. |
| Candle Filtration | Made up of clay, diatomaceous mud made by algae. | These filters have lengthy pores, trap the microbes throughout the length of the candle. |
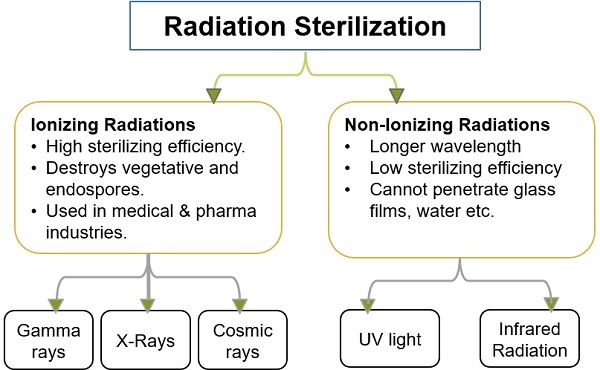
Radiation Sterilization
Radiations are lethal to living entities because they can infiltrate the cell, damaging nuclear material and essential biological macromolecules. The object to be sterilised is exposed to direct radiation during the radiation therapy process. As a result, all microbiological contamination on the surface is destroyed.
Although it is a very successful procedure, it has the potential to generate unwanted mutations, DNA breakage, or depolymerisation in those who use it. Therefore, you need to wear specialised safety gadgets while operating this technique.
Chemical Sterilization
It is preferred for items that are vulnerable to heat and radiation. Chemical sterilization is commonly accomplished by immersing the apparatus, tools, and equipment in a liquid sterilant. This kill both the microorganisms and the spores they produce. As these sterilants can be hazardous to humans, thus this approach must be closely regulated.
The biggest downside of this procedure is that the equipment frequently reacts chemically with the sterilant, causing damage to its composition.
Examples of some chemical sterilant
Ortho-phthalaldehyde (OPA): It has a fast-acting antimicrobial activity. With 12 hours of immersion time, 0.55 per cent of OPA concentration is deemed optimum. It’s a reusable item that doesn’t emit any noxious odours after use.
Glutaraldehyde: To destroy all types of spores and microbiological contaminants, it requires a more extended immersion period (approx. 22 hours). This is because it has a low penetration efficiency. As a result, its application is restricted to low-contamination zones.
Gaseous Sterilization
This method of sterilization involves the treatment of objects with the chemical sterilant in gaseous form or vapour state. This method is advantageous since it does not involve heat exposure, which eliminates the risk of unintended damage. Due to the lack of moisture, the risk of corrosion or chemical reaction is also reduced.
Plasma gas sterilization: Inside the confined chamber, vaporised H2O2 gas plasma is used to disinfect the apparatus, equipment and tools. All of the microbial life on the surface is destroyed as soon as the gas is released inside. The technique is environmentally benign and safe because it produces water and oxygen as by-products. Although it ensures full sterilization, it is quite costly due to the specialised and delicate machinery used.
Key Differences Between Disinfection and Sterilization
- Disinfection is an uncomplicated method that can be used anytime, anywhere and by anyone. Not very much technicality is essential for disinfection purposes.
On the other hand, sterilization is a complex and time-consuming procedure that necessitates specialised knowledge, scientific equipment, and other resources. - Disinfection promises to reduce the number of germs to safe levels where there is no risk of infection. However, sterilization ensures complete removal of the microbiome from the inside and outside of the object necessary for surgical operations, laboratory testing and R & D experiments.
- Disinfection is frequently used in the basic cleaning of floors and surfaces in households, hospitals and industries. Whereas sterilization is a typical technique that requires particular apparatus and tools to be efficiently done. Thus, it is performed for restricted purposes where complete decontamination is demanded.
- Sterilization ensures the destruction of all contaminants, but due to its technicalities, it becomes expensive. On the other hand, disinfection doesn’t demand any tools or machines thus; it is cheaper.
- Disinfection is a casual technique and therefore, there is no need to follow any specific protocol for it. But during sterilization, it becomes obligatory to abide by the strict protocol; otherwise, there is a risk of failure.
- Disinfection is capable of killing almost all microbiological creatures except vegetative spores and bacterial endospores. Sterilization is advantageous here as it kills all forms of microbes along with the spores.
Conclusion
The most important takeaway from the preceding information is that both approaches try to decontaminate the environment from undesired materials such as microorganisms, disease-causing pathogens and their spores. The sterilization proved to be a more potent mode because it can kill even the most difficult-to-kill spores. It is, nevertheless, usually favoured in hospitals and research facilities where contamination cannot be tolerated.
But, sterilization is not only costly and time-consuming, but it also exposes the product to serious harm after repeated usage. Disinfection, on the other hand, is a cost-effective and user-friendly approach for larger surfaces.
As a result, it becomes crucial to assess the scenario and determine which strategy is the best fit for you, as both have their own advantages and disadvantages.

Leave a Reply